Skid marks and fecal accidents can be a sign of...
Heather and her staff blog about all things pelvic health related
Including male, female, pediatric, transgender and nonbinary chronic pelvic pain, urinary dysfunction such as incontinence, prostatitis, sexual dysfunction, pregnancy, back pain, upcoming events and more.

All Blog Posts
Erectile Dysfunction Post Prostatectomy and How Pelvic Floor Therapy Can Help
Are You Experiencing Erectile Dysfunction Post...
How Can Physical Therapy Help Trans Women, Nonbinary, and Transfeminine People
This article explores how physical therapists...
How Can Physical Therapy Help Trans Men, Non-binary, and Transmasculine People?
Physical therapy for trans individuals is an...
How to Manage Discomfort After Low Intensity Shockwave Therapy
Softwave low intensity shockwave therapy is a...
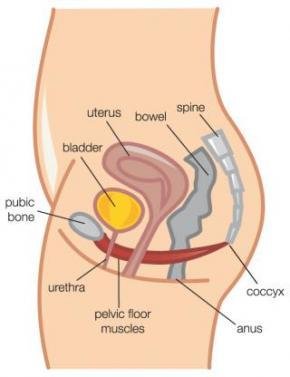
How Physical Therapy Eases Pelvic Floor Pain
Pelvic floor pain can be a tricky thing for many...
What is Low Intensity Extracorporeal Shockwave Therapy?
Read on to find out more about Low Intensity...
Effective Constipation Treatment: Evidence-Based Physical Therapy
Physical Therapy Can Play a Part in Effective...
Pelvic Floor Physical Therapy for Hemorrhoids and Anal Fissures – How it Can Help
When a Squatty Potty isn't Enough: How Pelvic...
Participate in a High Quality Study Using Shockwave Therapy for Painful Intercourse
Learn about low intensity shockwave therapy for...
Childhood Bedwetting and Genetics, What’s the Link & How to Treat it
Learn All About Childhood Bedwetting and...
Addressing Bladder Control for Your Child and Yourself
An In Depth Look at Bladder Control for Your...
Exercises to Benefit Aging: Best Exercises for Each Decade of Life
Best Exercise for Each Decade of Life: Exercises...
Heart Health = Hard Health: How Exercise Helps Sexual Dysfunction
There is growing research for the role of pelvic...
Endometriosis in Trans Men
Individuals affected by endometriosis often...
Updated Guidelines on Treating Interstitial Cystitis/Bladder Pain Syndrome
This month is Bladder Health awareness month and...
Spin The Right Way With the Help of a Therapist
Want to start a spin class? Afraid of returning...
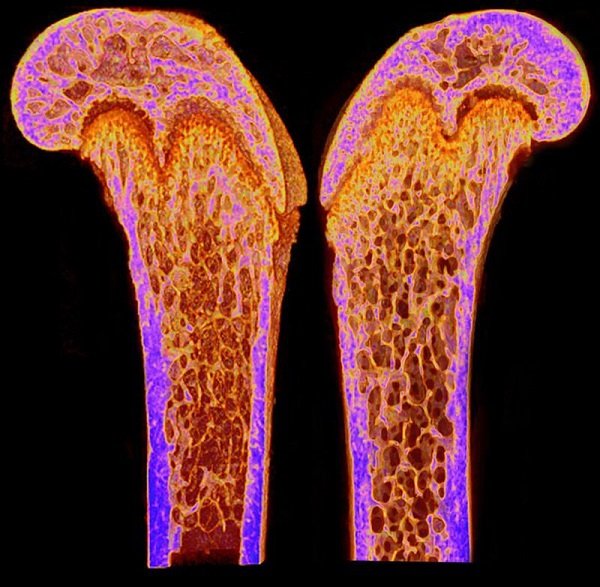
Osteoporosis Awareness Month: Bone Health and Prevention
May is Osteoporosis Awareness Month. Did...
Road to Boston Marathon Part 3: Building a Post-Run Recovery Routine
Building Your Own Post-run Recovery Routine A...
Road to Boston Marathon Part 2: Exercises for Marathon Runners
10 Strength, Conditioning, and Balance Exercises...
Boston Marathon Part 1: A Tribute to the First Female Runners in the Boston Marathon
Road to Boston Marathon Part 1 A Tribute to the...
Male Dysorgasmia: When Sex Hurts
Male Dysorgasmia is on the Rise In our practice,...
Gender-Affirming Surgeries: Post-Op Outcomes & Potential Complications
Over 1 million people in the United States...
Restless Legs Syndrome & Physical Therapy | Postpartum Recovery
Restless Legs Syndrome (or RLS) Restless legs...
What is IC and What Are The Symptoms? | Interstitial Cystitis
Restless Leg Syndrome (or RLS) Restless leg...
Men and LUTS | Causes & Treatments for Lower Urinary Tract Symptoms
Causes & Treatments for Lower Urinary Tract...
Grip Strength and Urinary Incontinence: The Unexpected Relationship
Is There Really a Relationship Between Grip...
The Link Between Urinary Incontinence and Low Back Pain | Fusion
It has long been recognized in the Pelvic...
Urinary Chronic Pelvic Pain and Resilience
A Recent Pilot Study Looked at the Connection...
Urinary Incontinence | Treatment & Products
Overview: Urinary Incontinence About 13 million...
Sexual Function After Cancer
This article introduces common unwanted side...
All About: Tarlov Cyst
This article will go over what a Tarlov cyst...
Highlight on Men’s Health: Incontinence
In this Blog Post We Highlight an Important...
Highlight: Mens Pelvic Pain
Highlight on Mens Pelvic Pain June is Men's...
Scoliosis Awareness! | Part 2: Scoliosis and the Pelvic Floor
Scoliosis and the Pelvic Floor - A Primer Part 2...
Functional Scoliosis and Structural Scoliosis | It’s Scoliosis Awareness Month!
An Overview of Functional Scoliosis and...
How Mindfulness Can Help with Erectile Dysfunction
Studies Have Shown that Mindfulness Can Help...
Histamines and Chronic Pelvic Pain, Chronic Prostatitis – the Connection
Research draws a connection between histamines...
Pediatrics and Pelvic Health: Bedwetting In Children – When is it a Problem?
Bedwetting In Children - When is it a problem? I...
Pediatrics and Pelvic Health: Chronic UTIs, Bowel and Bladder Dysfunction
Frequent Urinary Tract Infections (UTIs) in...
Male Pelvic Pain: What You Should Do If You Have a “Headache in Your Pelvis”
Did you know that chronic pelvic pain can happen...
Healthy Aging Month: Enjoying Sex With a Bad Back and Hips
September is Healthy Aging Month - Learn...
Male Sexual Dysfunction in Pelvic Cancer Survivors
A 2019 literature review by Twitchell et al....
Cycling and Erectile Dysfunction: The Connection
As an approved way to get exercise during the...
How Bladder Health Can Affect Prostate, Erectile Function, and Pelvic Health
Doctors have known for decades that smoking...
Pelvic Floor Therapy for Pubic Symphysis Pain
Are You Considering Pelvic Floor Therapy for...
How Pelvic Floor Therapy Can Help Erectile Dysfunction and Urinary Intontinence After Radical Prostatectomy
Radical prostatectomy is a procedure that is...
Finding The Right Personal Lubricant For You
When talking to some of my patients, I’ve...
Heather returns from work with the Chinese Olympic Committee
I just returned to Los Angeles after completing...
Why do my testicles hurt?
Asking Yourself "Why do my testicles hurt?" Read...
Is Your Bladder Cranky?! It Might Be Irritated
Did you know specific food and drinks can...
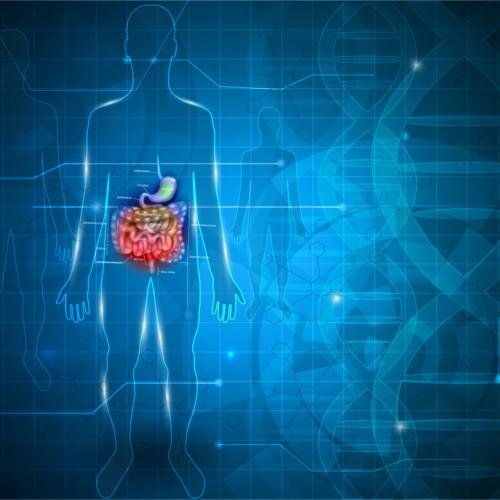
The Scoop on Poop – What is your poop telling you?
May is Pelvic Pain Awareness month and healthy...
Ready, Set, Cycle: How to fit your Bike Correctly
Did you know that riding a bike that doesn’t fit...
Back to School Series: Bookbags and Back aches
How to prevent back pain for your child With the...
Back to School Series: Pediatrics and the Pelvic Floor
Childhood Constipation and how Pelvic Floor...
Pediatric Incontinence and Pelvic Floor Dysfunction
While occasional daytime and nighttime accidents...
Evidence-Based Recommendations for Managing Prostatitis Related Pain: Healthy Sex and Lifestyle Habits
Managing Prostatitis Related Pain is Possible...
Yoga Therapy to Ease Prostatitis and Chronic Pelvic Pain
Did You Know That You Can Practice Yoga Therapy...
Evidence-Based Recommendations for Managing Prostatitis Related Pelvic Pain
Ways Prostatitis Related Pelvic Pain Can Be...
Nonbacterial Prostatitis: Chronic Pelvic Pain in Men
This article will review how prostatitis can...
Chronic Constipation 101
Most people experience occassional constipation....
What’s Up Down There, Doc?
Pelvic floor physical therapy is one of the best...
Why You Should STOP Doing Kegels NOW
In my last post, “Why You Should Be Doing Kegels...
Official Book Release Today!
I am proud to announce the official book release...
Why you should be doing Kegels RIGHT NOW!
Wondering Why You Should be Doing Kegels? Read...
What are Kegels?
What are Kegels? Kegels are a contraction of a...
Featured on the Blog
How do you know when it’s wise to go running after having a baby?
As an expert in the field of all facets of postpartum care, I believe that a measured approach to exercise is vitally important to achieve optimum pelvic health without complications, and Daniella so graciously states in the opening paragraph of her article:
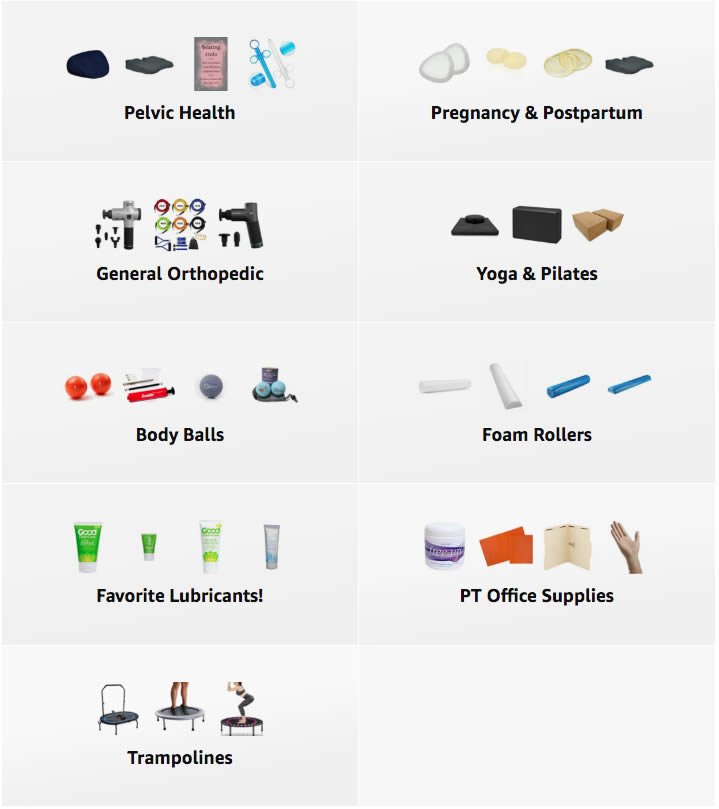
Products We Love
Amazon
A Curated List of Excellent Items at Amazon
From books and workout accessories to general othopedic items and even personal lubricants!
When you visit our space on Amazon you will find a wide variety of products that will help in your quest to not just better pelvic health, but to your overall health and wellbeing too! Click anywhere in this ad to go there now and find what you need!
SRC Health
Designed by women for women.
Whilst recovering in hospital after the birth of her first child, our founder Sinead O’Donovan decided that new mums deserved more help getting back to their busy lives. Drawing on her extensive medical and bio-mechanical background, Sinead envisaged a garment that would be comfortable for new mums to wear all day whilst giving her all the support she and her body need.

In Heather’s own words:
I thought it’s finally time to share one of my post-op recovery secrets — I’ve been loving that supported life in my @srchealth compression leggings since my hip labral repair surgery last October. When I wear them, my chronic left SI joint hurts less and my legs feel like they’re being micro-massaged all day long!
Click here to shop the full SRC Health line, and use code FEMINA at checkout for special pricing!
MedAmour Body Safe Products and Services
Designed by women for women.
Whilst recovering in hospital after the birth of her first child, our founder Sinead O’Donovan decided that new mums deserved more help getting back to their busy lives. Drawing on her extensive medical and bio-mechanical background, Sinead envisaged a garment that would be comfortable for new mums to wear all day whilst giving her all the support she and her body need.

Click here and use code FEMINAPT to save $10 off your first $50 purchased.