Search Our Site
Popular Topics
Meet Our Team
About Heather Jeffcoat, DPT | Los Angeles Pelvic Floor Doctor


Heather and her staff blog about all things pelvic health related
Including male, female, pediatric, transgender and nonbinary chronic pelvic pain, urinary dysfunction such as incontinence, prostatitis, sexual dysfunction, pregnancy, back pain, upcoming events and more.
- Details
- Kasia Gondek, PT, DPT, CSCS
- 1965
10 Strength, Conditioning, and Balance Exercises for Marathon Runners
Leading up to the Boston Marathon, I have been incorporating these 10 key exercises into my weekly routine (3x/week) to keep my body strong and balanced. Check out videos of these exercises here (link to instagram post). These exercises target the key muscle groups used by runners. These are for educational purposes, not meant to treat medical conditions nor supplement medical advice.
Mat-based Strength and Conditioning for Boston
- Details
- Kasia Gondek, PT, DPT, CSCS
- 1801
Road to Boston Marathon Part 1
A Tribute to the First Female Runners in the Boston Marathon
On April 18, 2022 I am excited and grateful to be able to run the historic and prestigious Boston Marathon! As a physical therapist at Fusion Wellness /Femina Physical Therapy and avid long-distance runner for over 20 years, I’m excited to share my training journey with you leading up to the race. This race holds a special place in the hearts of long-distance runners because you must run a qualifying race with a qualifying time. Females ages 18-34 must run 3 hours 30 minutes or better, and males ages 18-34 must run 3 hours flat or better.
- Details
- Kasia Gondek, PT, DPT, CSCS
- 1727
Over 1 million people in the United States self-identify as transgender, and according to the 2019 Plastic Surgery Statistics by the American Society of Plastic Surgeons, around 11,000 gender confirmation surgeries were performed annually in the U.S. Gender-affirming (also referred to as sex-affirming or gender-confirming) surgery encompasses various elective plastic surgery procedures that result in physical characteristics typically associated with being male or female. While not the case for all people who identify as transgender, some people experience distress that their sex assigned at birth does not match their gender identity (termed gender dysphoria). These procedures are just one means to help someone feel congruence between their gender identity and physical traits associated with a particular sex. It is important to note that just because a person identifies as trans-gender or non-binary does not mean that they feel gender dysphoria, nor does it imply that they need or want medical procedures or surgeries to look more feminine or masculine.
Types of Gender-Affirming Surgeries:
Gender-affirming surgeries can involve the face, chest, or genitalia, and are listed in the table here:
- Details
- Staff
- 5307
Restless Leg Syndrome (or RLS)
Restless leg syndrome (or RLS) is a condition where there are uncontrollable urges to move limbs (mostly in the legs, but sometimes in the arms) that follows a circadian pattern, namely evenings/overnight when resting.
The urges usually come with unpleasant sensations such as tingling, burning, itching, or otherwise painful. Restless leg syndrome can often be alleviated by movement, but as you can imagine, it can be debilitating and impair sleep, and thus quality of life. It is common to experience mood swings, anxiety and depression. It is estimated that about 3.9-14.3% of the general population suffer from RLS. It is the most common movement disorder in pregnant women. There is either primary (idiopathic) RLS, or secondary (acquired) RLS due to pregnancy, renal pathologies and are also associated with diabetes, hypertension and other metabolic conditions. The two most common risk factors for RLS are iron deficiency and kidney disease.
- Details
- Staff
- 2612
Interstitial cystitis (IC) also known as bladder pain syndrome or painful bladder syndrome, is a debilitating condition that significantly affects the quality of life of patients living with it.
Symptoms of IC include:
- An unpleasant sensation (pain, pressure, discomfort) perceived to be related to the urinary bladder >6 weeks in duration6,7,9
- Increased pain with specific foods or drinks and/or worsened with bladder filling and/or improved with urination9.
- Urinary urgency (Seen in 84% of IC patients)6.
- Urinary frequency (>10x/day) (Seen in 92% of IC patients)6.
- Details
- Staff
- 3896
Causes & Treatments for Lower Urinary Tract Symptoms
Men may experience different types of lower urinary tract symptoms (LUTS)
Men may experience different types of lower urinary tract symptoms (LUTS) and are often divided into different categories: storage symptoms (urinary urgency, frequency, nighttime peeing, incontinence), voiding symptoms (painful urination, incomplete emptying, dribbling, poor urinary stream), and/or post voiding symptoms (post-void dribbling, pain after urination, etc.).
Living with these symptoms can be debilitating and significantly decrease quality of life. Between 70-90% of older men over 80 experience some version of LUTS. LUTS are often associated with bladder outlet/obstruction issues due to enlarged prostate. However, this is not always the case and can arise from other bladder or urethra disorders including overactive bladder syndrome, painful bladder syndrome, chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS), and other.
- Details
- Staff
- 2084
Is There Really a Relationship Between Grip Strength and Urinary Incontinence?
Read on to find out1
At Fusion Wellness & Physical Therapy, we take pride in understanding and applying how your whole body affects your pelvic health. In this article, we explore how urinary incontinence and other bladder issues are correlated with grip strength.
A study conducted at the Jeju National University measured grip strength in patients and found statistically significant differences in patients with incontinence, overactive bladder and nocturia4. They found these patients had a weaker grip strength (less than 18kg) using a hand dynamometer.
- Details
- Staff
- 3078
It has long been recognized in the Pelvic Physical Therapy World that there is a connection between urinary incontinence and low back pain.
Clinically, we often see patients that come in with both symptoms. How common is urinary incontinence among people also affected by low back pain? What comes first, the urinary incontinence or the back pain? What causes this?
In a recent systematic review, a positive association of 83% was found between urinary incontinence and low back pain or pelvic girdle pain. Pelvic girdle pain is defined as the area below the low back and below the abdomen (gluteal region in the back and pubic bone in the front). The strength of this correlation depends on many factors such as type of urinary incontinence, pain severity, and length of pain.
- Details
- Staff
- 2793
A Recent Pilot Study Looked at the Connection Between Urinary Chronic Pelvic Pain and Resilience
A recent pilot study looked at how resilience affects patients with urinary chronic pelvic pain (UCPP) conditions and chronic overlapping pain conditions (COPCs).
Resilience can be defined as the “capacity to adapt successfully to disturbances that threaten a patient's viability, function or development.” (Southwick et al., 2014)
Resilience is now an important aspect in the treatment of pain, as it can increase psychosocial well‐being and the quality of life in patients living with chronic pain. (Casale et al., 2019)
- Details
- Staff
- 2491
Overview: Urinary Incontinence
About 13 million people in the United States experience some type of incontinence, or unwanted leakage of urine. More than 50% of women over 20 years old reported experiencing urinary incontinence at some point in their lives. Moderate to severe urinary incontinence is prevalent in 17% of women aged 20 years or older, but more commonly occurs in 38% of women aged 60 years or older.
Types of Urinary Incontinence
Stress Urinary Incontinence
Stress urinary incontinence is when leakage occurs during stress-induced activities such as exercises, coughs, and sneezes.
- Details
- Staff
- 3691
This article introduces common unwanted side effects that affect sexual function after cancer and discusses strategies to counteract these symptoms.
Sexuality can be a big part of who we are as individuals.
Sexual functioning can be defined as “specific physical, physiological, neurological and emotional behaviors expressed by an individual response” (Wood, 1984).
Certain cancers can unfortunately affect our sexual health, including cervical, ovarian, bladder, kidney, colorectal and breast cancer to name a few.
Some cancer treatments can cause unwanted side effects that affect our sexual health such as decreased sexual arousal or desire, vaginal stenosis (narrowing of the vaginal canal), dyspareunia (painful sexual intercourse), and bladder/bowel dysfunction. Issues with sexual function after cancer can affect our relationships with ourselves and with our partners, and reduce quality of life. Hopefully a physical therapist is part of your team to help guide you during this challenging time and minimize these aforementioned side effects. Otherwise, ask for a pelvic floor physical therapist to join your team during your recovery!
- Details
- Staff
- 23748
This article will go over what a Tarlov cyst is, what symptoms can arise from having a Tarlov cyst, how it is diagnosed, and common conservative and surgical treatments.
What is a Tarlov Cyst?
Tarlov cysts are sacral perineural cysts that consist of cerebrospinal fluid (CSF) close to the dorsal root ganglion on our sacral spine (the triangle shaped bone that connects to our tailbone). Tarlov cysts are often incidental findings on MRI’s, meaning most people with no symptoms may have Tarlov cyst(s). Paulsen, et al, looked at 500 MRIs of the lumbosacral spine and found an incidental rate of 4.6%; of which 20% were symptomatic. Approximately 1% of the cysts are large enough to cause compression, thus requiring prompt treatment.
- Details
- Staff
- 3722
Highlight on Mens Pelvic Pain
June is Men's Health Month
Pelvic health is not only tied to females; males also experience pain in their pelvis including their bladder and rectum, but may also extend to their testicles, penis, prostate, etc. Common mens pelvic pain diagnoses include (but not limited to):
- Details
- Staff
- 2076
In this Blog Post We Highlight an Important Aspect of Mens Health: Incontinence
Although it is more common to experience urinary incontinence in females compared to men, men can still experience urinary incontinence.
Just like females, males also have a pelvic floor that controls the sphincters to either contract or release (for holding in urine or releasing urine, respectively). When there is dysfunction or coordination issue (whether it is weakness or too tight) in the pelvic floor, incontinence can occur. The CDC estimates that almost 44% of men in the US who are not in an institution struggle with urinary incontinence.
- Details
- Staff
- 7282
Scoliosis and the Pelvic Floor - A Primer
Part 2 of our Series on Scoliosis Awareness
June is Scoliosis Awareness Month! If you recall from part 1, scoliosis is a 3-D curvature of the spine. Some people get it in early childhood or adolescence, and others get it as an adult. This can lead to low back pain, breathing difficulties, and … affect the function of the pelvic floor muscles!





































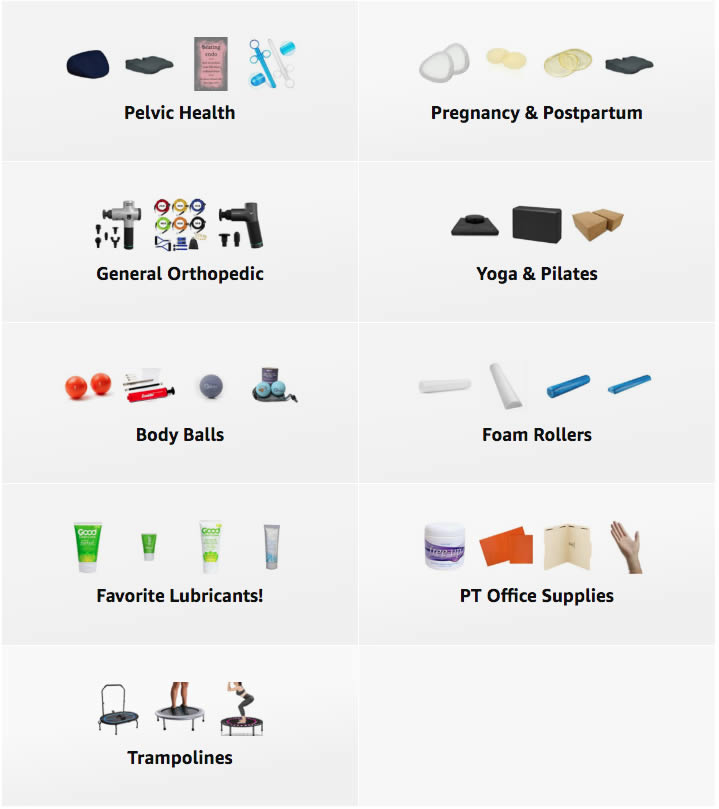 A Curated List of Excellent Items at Amazon
A Curated List of Excellent Items at Amazon