Vaginismus:
Vaginismus definition: the involuntary muscle spasms involving the superficial pelvic floor muscles that typically cause painful entry, limiting or preventing intercourse, tampon insertion or pelvic exams. Many women will also describe “a wall” that limits penetration, that may or may not be painful. This is not a lifelong condition and can be cured. The most successful vaginismus treatment is a combination of manual treatment, corrective exercises and home instruction. Most women will use vaginal dilators as a part of their home program to treat vaginismus. More information on our female-based services can be found on our women’s program website at Femina Physical Therapy. Click here for more information on vaginismus.
Vulvodynia:
Vulvodynia is defined as “vulvar pain” or pain of the external female genital region. Symptoms include burning, stinging, and irritation of the tissues in this region. Light touch or pressure can cause severe pain with sitting, walking, riding a bicycle, and sexual intercourse. There are many subtypes of vulvodynia, including vestibulodynia, vulvar vestibulities and clitorodynia. More information on Vulvodynia can be found on our women’s services site here.
Vulvar Vestibulitis / Vestibulodynia:
Vulvar Vestibulitis/Vestibulodynia is a subtype of vulvodynia with tenderness specific to the vulvar vestibule. This occurs with pressure to the site that causes pain at the vulvar vestibule with touch or attempted penetration. Tissues may be red or swollen at times. Vulvar vestibulitis is used when there is inflammation present at the vestibule. Vestibulodynia strictly refers to pain at the vestibule. Vestibuloydynia may be further subclassified as Provoked or Unprovoked. Provoked vestibulodynia refers to pain that occurs with a pressure applied to the area. Unprovoked vestibulodynia refers to pain that occurs in the absence of a direct pressure applied. All subtypes can lead to vaginismus, so need to be treated simultaneously for an optimal outcome.
Endometriosis:
When endometrial-like tissue grows outside of the uterus, an inflammatory cycle is set up, scar tissue before begins to form and both of these things can effect bowel, bladder and sexual function. This chronic cycle of inflammation can also lead to muscle guarding, pelvic pain, postural changes, decreased activity and in severe cases, social withdrawal. 1 in 10 women have endometriosis, and 70% of girls with painful menstrual cramps also have endometriosis. Specialized physical therapy that addresses the complete picture of pelvic floor dysfunction, orthopedic issues and visceral restrictions is one of the main tools to help minimize the effects of endometriosis on your body. Read some of our many blogs on endo on our female based services website Femina Physical Therapy, including one of owner Heather Jeffcoat’s favorites: Teaching Your Daughters About Endometriosis.
Interstitial Cystitis / Painful Bladder Syndrome
Painful Bladder Syndrome (formerly known of as Interstitial Cystitis) is a pelvic pain, pressure, or discomfort related to the bladder, typically associated with persistent urge to void or urinary frequency, in the absence of infection or other pathology. An out-dated definition characterized the disorder as uroepithelial inflammation and/or hypersensitivity of bladder afferent nerves, however bladder inflammation is rarely found, and Hunner’s Lesions occur less than 8% of the time. Much more understanding of interstitial cystitis / painful bladder syndrome has occured since 2007, and in 2014, the American Urology Association updated their guidelines for Interstitial Cystitis treatment to include Pelvic Floor Physical Therapy as one of the top line treatments for this disorder. Signs and symptoms can include perineal pain, frequent urination, feeling like you have to pee even though you just went, the strong urge to pee without much volume coming out. Patients typically have a history of taking many rounds of antibiotics with little to no help in their symptoms.
Prostatitis:
Prostatitis includes acute or chronic bacterial or non-bacterial inflammation in the epididymis of the male genitalia. Signs and symptoms can include prostate or perineal pain, difficulty with urination, urinary retention and hesitancy, urinary urgency, frequent urination and decreased urine stream. Like interstital cystitis / painful bladder syndrome, patients typically have a history of taking many rounds of antibiotics with little to no help in their symptoms. Another name this is often referred to is nonbacterial prostatitis, and pelvic floor physical therapy is one of it’s top line treatments.
Pudendal Neuralgia:
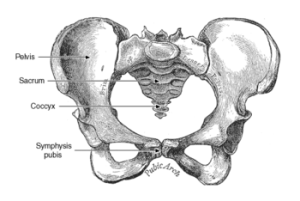
Pudendal neuralgia is severe, sharp pain along the course of the pudendal nerve. There are five essential criteria for diagnosis of pudendal neuralgia:
- Pain in the anatomical territory of the pudendal nerve
- Worsened by sitting
- The patient is not woken at night by the pain
- No objective sensory loss on clinical examination
- Positive anesthetic pudendal nerve block.
Other criteria that are considered complimentary include: burning, shooting, stabbing pain or numbness, allodynia, sensation of a rectal or vaginal foreign body (sympathalgia), worsening of the pain during the day, pain predominantly on one side, pain triggered by bowel movements, and tenderness to palpation along the ischial spine (on clinical exam).
Associated signs and symptoms that may also be present are: buttock pain on sitting, referred sciatic pain, pain referred to the medial aspect of the thigh, suprapubic pain (pain above the pubic bone), frequent urination, pain with a full bladder, pain occurring after ejaculation, pain during or after intercourse (dyspareunia), erectile dysfunction.
Treatments for Female, Male, Transgender and Gender Expansive Patients with Sexual Dysfunction:
Pelvic floor muscles are very important in the physiology of an individual’s sexual response. Physical therapists play an important role in the multidisciplinary team when dealing with sexual dysfunctions. Arousal and orgasmic disorders, erectile dysfunctions, and ejaculatory dysfunctions and sexual pain are areas that pelvic floor physical therapy specialists can assist patients in restoring sexual health and pleasure. Don’t see your diagnosis or description of pain on our lists? Sometimes new terminology is coming up for conditions we’ve been treating for years, and we do our best to keep our website up to date. Feel free to call to speak with one of our therapists and we can better determine if we are the right office for you.
- To see our full list of Male Sexual Dysfunctions we treat, click here.
- To see our full list of Female Sexual Dysfunctions we treat, click here and you’ll go to our Female services brand, Femina PT.
- To read more about how we treat transgender and gender expansive patients, click here.